Immune-Mediated Inflammatory Diseases
Immune-mediated inflammatory diseases (IMIDs) constitute a group of diverse but prevalent disorders – seen in 5-7 % of the western population –that are characterized by an alteration in cellular homeostasis, driven by common immune and genetic pathways. Different IMIDs affect various parts of the body, however, systemic involvement is commonly seen in all of these conditions, causing significant morbidity, mortality, and economic loss. It is well known that both environmental factors – including smoking, diet, drugs, geographical and social status, stress, and infectious agents – and genetics play a central role in the pathogenesis of IMIDs. Genome-wide association studies and single-nucleotide polymorphism scans have recently led to the identification of genes commonly found in different IMIDs, as well as those that are disease specific. In the current clinical scenario this group of diseases is not completely curable, however, targeted monoclonal antibodies and biologic therapies are offering great promise as therapeutic strategies compared to the previously accepted option of blanket immunosuppression. IMIDs include rheumatoid arthritis, the spondylarthritis disease spectrum, connective tissue disorders, cutaneous inflammatory conditions – including psoriasis and atopic dermatitis – inflammatory bowel disease, asthma, and autoimmune neurological diseases such as multiple sclerosis.1, 2
Sources and Strategies for Treatment
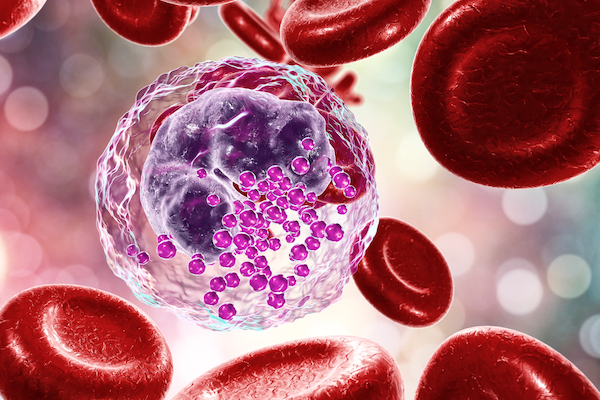
The immunopathogenesis for most IMIDs is orchestrated by the CD4+ T lymphocytes. The Th 1 subset exerts proinflammatory effects – via TNFα, IL-6, IL-1 – and the Th 2 subset is known to have a protective or an anti-inflammatory effect via IL-4 and IL-10. In addition, strategies targeting the Th17 axis either by blocking the IL-17 directly or by preventing Th17 cell differentiation have proven to have superior efficacy in the management of IMIDs, validating the role of the TH17 axis in the development of these disorders. In addition to T cells, B cells also contribute to immune complex formation and complement activation in the development of IMIDs. This is demonstrated by the success of B- cell depletion therapy in the treatment of rheumatoid arthritis, for example.1, 2, 3
The fact that IMIDs share immune dysregulation pathways has led to the development of mechanism-based treatments that are now replacing the more traditional symptom-management methods2. Immunotherapeutic approaches broadly have two domains – cell-based and agent-based, using immunomodulators, such as cytokines and antibodies – that aim to restore or augment the functioning of the immune system. The key extracellular, membrane-bound, and intracellular targets for biological and small-molecule therapies that have transformed the landscape in the management of IMIDs are:3
| Extracellular targets | IL-12/23p40, IL-23p19, IL-17A, IL-17F, TNF, IL-1, IL-6, IL-6R, GM-CSF, IL-4, IL-5, IL-13, IFNɣ, BLyS |
|---|---|
| Membrane targets | CD22, CD20, α4 integrins, IL-17RA, tmTNF, IL-6R, IFNR, IL-4R, IgE, CD80/86, S1PR1 |
| Intracellular targets | JAK1, JAK2, JAK3, TYK2, PDE4, BTK |
Despite recent advances, these approaches are still not achieving adequate long-term remission, let alone a cure, for IMIDs. Inflammatory pathways are distinct from pain pathways and, therefore, even biologics are not proving fully successful in the management of individual patients. As well as those listed above, there is currently a further range of targets in clinical trials. Other strategies, such as the use of stem cells, modified regulatory T cells, chimeric antigen receptor T cells, and tolerized dendritic cells, also offer potential. In conclusion, biological and small-molecule-based therapies represent an exciting phase in the treatment of IMIDs, but the challenge remains to identify when to introduce biologics to arrest the progression of the disease in the early phase. Interventions during the pre-disease state in susceptible individuals is certainly an area to explore for designing newer therapies.3
References
1. García, M.J., Pascual, M., Del Pozo, C. et al. (2020). Impact of immune-mediated diseases in inflammatory bowel disease and implications in the therapeutic approach. Sci Rep 10, 10731. https://doi.org/10.1038/s41598-020-67710-2
2. Kuek, A., Hazleman, B. L., & Ostör, A. J. (2007). Immune-mediated inflammatory diseases (IMIDs) and biologic therapy: a medical revolution. Postgraduate medical journal, 83(978), 251–260. https://doi.org/10.1136/pgmj.2006.052688
3. McInnes, I.B., Gravallese. (2021). E.M. Immune-mediated inflammatory disease therapeutics: past, present and future. Nat Rev Immunol 21, 680–686. https://doi.org/10.1038/s41577-021-00603-1

