Diseases of the Microbiome
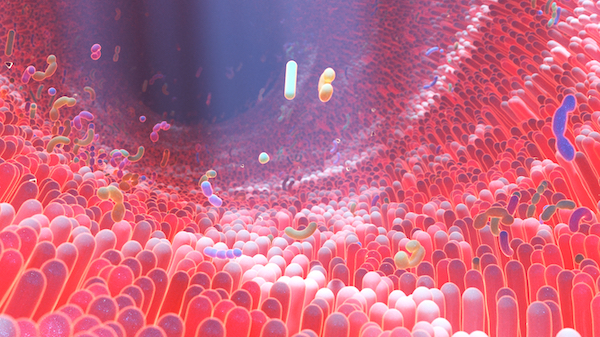
The human body is a natural habitat for more than 100 trillion microbes, including bacteria, archaea, viruses, and eukaryotic microbes. The complex interactions between intestinal microbiota and a host impact many physiological processes and contribute to the development and progression of a wide spectrum of diseases. Commensal bacteria colonize the human gut shortly after birth, evolving gradually into a diverse ecosystem and eventually developing a symbiotic relationship with the body. Microbiota research has increased significantly in recent years, largely thanks to advances in techniques – such as 16S rRNA sequencing, whole genome sequencing, metabolomics, and proteomics, combined with computational-based bioinformatics analysis – that have unearthed links to so many underlying metabolic processes.
The microbiota expresses around 150 times more genes than the entire human genome, and its composition varies according to the location, age, gender, race, and diet of the host. It is now known that gut microbes modulate the metabolic phenotype, carry out xenobiotic processing, regulate epithelial development, maintain energy homeostasis, and influence innate immunity, and they may also be associated with more regulatory processes that are not known yet.
Sources and Strategies for Treatment
Dysbiosis of gut-colonizing bacteria has been linked to the pathogenesis of several diseases, although the mechanisms behind this are not yet clear. These include:
- Metabolic disorders – type 2 diabetes mellitus and obesity: a lower diversity and a higher resilience of microbes resulting from complex gene-diet-environment interactions are implicated in inducing inflammatory changes, altering appetite signaling, and causing insulin resistance in the host. Emerging evidence points towards the ingestion of specific fibers or therapeutic microbes as promising strategies to combat dysbiosis and improve functioning of metabolic pathways.
- Infectious diseases: infections significantly alter the microbiome of the gut and vice versa. In addition, the widespread use of antibiotics and immunosuppressive drugs also affects the balance of the microbiota. The course of bacterial infections such as C. difficile, H.pylori, and certain viral infections, including HIV and hepatitis B, is also reported to be partly dependent on gut health.1, 2
- Liver diseases: chronic exposure of the liver to gut-derived factors, including bacterial endotoxins and bacterial components, may influence liver function and contribute to the pathogenesis of liver cirrhosis, spontaneous bacterial peritonitis, and hepatic encephalopathy. Maintaining a normal microbial community using probiotics and prebiotics could help to improve treatment or preventive strategies for liver diseases.3. 4
- Allergic diseases: the interaction of gut microbiota with the immune system during infancy and childhood provides signals that promote the maturation of antigen-presenting cells (APCs) and regulatory T-cells (Tregs), which are key in the development of immunologic tolerance. Altered microbiome diversity has been implicated in the resolution of cow’s milk allergy and, conversely, increased susceptibility to allergic asthma.
- Psychiatric disorders: the newly recognized microbiota-gut-brain axis involving immune, hormonal, and neural pathways may disrupt homeostasis in the host and participate in the manifestation of autism or major depressive disorders by causing the release of inflammatory cytokines, and activating the vagus nerve and spinal afferent neurons.
- Cancers: there is emerging evidence that the local microbiota in the tumor microenvironment – especially in cancers arising from mucosal sites – is tumor-type specific and may directly regulate cancer initiation, progression and responses to therapy.5 The specific role of the microbiota in some cancers is better understood including:
- Esophageal cancer: Long-term changes in esophageal microecology due to frequent exposure to antibiotics may lead to a higher incidence of esophageal reflux and eventually esophageal adenocarcinoma (EA). The role of H. pylori, although widely researched, is still unclear, with some studies suggesting a protective role in the development of EA.
- Colorectal cancer: Many bacteria-derived metabolites, including short-chain fatty acids, and a high fiber intake have been implicated in the suppression of colon cancer development by inducing apoptosis, altering gene expression, and modulating inflammatory responses and cytokine levels. Regulation of the gut microbiome through dietary control or antibiotic treatment may offer potential therapeutic benefits.6
Amplicon sequencing of 16S ribosomal RNA regions is a standard technique used to assess microbial diversity, but its applications are limited as the eukaryotic and viral components of the microbiome are not captured. Whole-genome sequencing can provide information on strain-to-strain variations, and this can be used to determine the characteristic pathogenicity, toxins, virulence factors, epitopes, and antibiotic resistance properties of the microbiome, unraveling the complex interactions of microbes within a community. In addition, miniaturizing sequencing workflows with automated liquid handling systems can further help in reducing operational costs and risks of contamination, offering high quality and consistent methods to create sequencing libraries.7
Related Content
References
1. Pham TA, Lawley TD. (2014) Emerging insights on intestinal dysbiosis during bacterial infections. Curr Opin Microbiol. 17(100):67-74. doi: 10.1016/j.mib.2013.12.002
2. Harper A, Vijayakumar V, et al (2021). Viral Infections, the Microbiome, and Probiotics. Front Cell Infect Microbiol. 12(10):596166. doi: 10.3389/fcimb.2020.596166
3. Xu S, Zhao M, et al. (2021) Effectiveness of Probiotics and Prebiotics Against Acute Liver Injury: A Meta-Analysis. Front Med (Lausanne). 21(8):739337. doi: 10.3389/fmed.2021.739337
4. Chen HT, Huang HL, et al. (2020). Therapeutic advances in non-alcoholic fatty liver disease: A microbiota-centered view. World J Gastroenterol. 26(16):1901-1911. doi:10.3748/wjg.v26.i16.1901
5. Wong-Rolle A, Wei HK, et al. (2021) Unexpected guests in the tumor microenvironment: microbiome in cancer. Protein Cell. 12(5):426-435. doi: 10.1007/s13238-020-00813-8
6. Wang B, Yao M et al. (2017). The Human Microbiota in Health and Disease. Engineering. 3(1):71-82. doi:10.1016/J.ENG.2017.01.008
7. Lai J, Hutto S et al. (2019). Whole Genome Sequencing of Microbial Communities for Scaling Microbiome and Metagenomic Studies. Journal of Biomolecular Techniques : JBT, 30(Suppl), S41.

